
Raised bilirubin levels in the body, or hyperbilirubinaemia, is common in the first week of life, affecting 50%–70% of term babies and 80% of preterm babies.( 3- 5) Up to 30%–40% of predominantly breastfed babies may still be jaundiced at the age of 3–4 weeks.( 6) Breast milk jaundice is a common type of unconjugated hyperbilirubinaemia( 7, 8) that may occur in the second or third week of life. Unconjugated bilirubin is metabolised in the liver to produce conjugated (or ‘direct’) bilirubin, which passes into the gut and is largely excreted in stool.( 1) HOW RELEVANT IS THIS TO MY PRACTICE? Most of the unconjugated (or ‘indirect’) bilirubin formed is bound to albumin as it circulates, although some bilirubin is ‘free’ and hence able to enter the brain.
resolving cephalohaematoma), infections, liver disease, bruising and metabolic disorders.( 1) Glucose-6-phosphate dehydrogenase (G6PD) deficiency is one common cause of severe neonatal jaundice in Singapore.( 2) Bilirubin is mainly produced by the breakdown of red blood cells. Neonatal jaundice, which refers to jaundice during the early days of life, has many aetiologies, including maternal and fetal blood group incompatibility (most commonly Rhesus or ABO incompatibility), certain causes of haemolysis (e.g.
#Pathological jaundice newborn 24 hours after birth skin#
Patients present with yellow colouration of the skin and whites of the eyes.

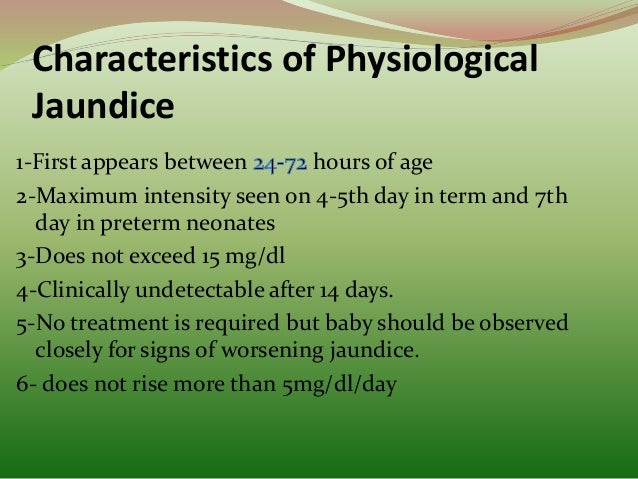
Jaundice refers to a condition caused by the accumulation of bilirubin in the skin, mucous membranes and sclerae. Mrs Tan wanted advice on what else she could do to improve Michael’s jaundice and whether exposure to the sun would help. You asked how Michael had adjusted and how everyone at home had adapted to their new roles since the birth. You reviewed the child’s health booklet and noticed that his total serum bilirubin level, from the afternoon of the day before their visit, was 119 µmol/L (7 mg/dL). She provided a letter of discharge from the hospital where Michael was delivered. Mrs Tan took her three-day-old child, Michael, to your clinic for a review of his neonatal jaundice. The importance of stool colour examination and its role in early detection of cholestatic jaundice is emphasised. They include clinical assessment of the baby’s well-being looking out for features that suggest pathological jaundice assessment for the presence of high-risk features utilising appropriate laboratory tests for monitoring assessing the degree of jaundice to decide if the child can be safely followed up in primary care and providing advice on primary prevention measures and allaying parental concerns. This article describes consultation tasks in the primary care setting with the aim of providing a guide for the safe management of neonatal jaundice. High levels of serum bilirubin can also result in bilirubin encephalopathy. However, others have pathological jaundice, which must be detected early. Most afflicted babies have physiological jaundice and their prognosis is good.

Neonatal jaundice is a common condition seen in the primary care setting.


 0 kommentar(er)
0 kommentar(er)
